More is at stake than just finding a cure
Over the past 30 years medical research on the human immunodeficiency virus (HIV) has taken giant steps forwards. These days one pill is enough to keep infection under control. But there is no cure in sight, and discrimination is still common.
“You do not recover from HIV,” said Enos Bernasconi, deputy head of internal medicine at Lugano’s regional hospital. “But most people who follow a course of treatment with antiretroviral drugs can lead a normal life and have children.”
The Swiss HIV Cohort Study, which brings together large-scale epidemiological data, has shown that in 90 per cent of infected patients undergoing therapy, the virus is no longer measurable in the blood.
“Up till a few years ago we were managing 70 per cent at most,” pointed out Bernasconi, who has been working on HIV and infectious diseases for over two decades. If patients get appropriate treatment he added, “we are able to control the infection over the long term”.
Research pushes forward
HIV therapy now uses drugs that inhibit virus replication. This puts the brakes on the opportunistic, and often fatal, infections that are the hallmarks of Aids. “But early treatment is essential, and to ensure one takes the medication,” cautioned Bernasconi.
Medical research is currently focused on perfecting antiretroviral drugs.
“For two or three years now they have been developing tritherapies in a single tablet. This has meant a big improvement for the patient,” said Bernasconi, who was recently appointed the medical faculty at Geneva University, one of the main HIV research centres in Switzerland.
Researchers are also trying to prevent side-effects of the treatment such as allergic reactions, kidney and liver problems. “This is of fundamental importance. In the past we have often had to break off a treatment because of intolerance to a particular drug,” added Bernasconi.
Antiretroviral drugs can also stop the infection from settling in after exposure to the virus, he said: “They can be given to healthcare workers who prick themselves by accident with an infected needle. In such cases a month’s course of treatment will do the job.”
This summer, the US approved the sale of Truvada, the first drug able to prevent HIV infection. This is a prophylactic aimed at healthy individuals who are at risk, such as those who have sex with infected partners.
But extending the use of antiretroviral drugs to healthy individuals is “debatable”, said Bernasconi. “Even if the studies do not show it, this ‘uncontrolled’ use could lead to an increase in resistance. So we should be asking ourselves if it’s a good idea to be giving drugs to people who are not sick,” he pointed out.
A vaccine is still way off too, he warned: “There is worthwhile progress being made, but there isn’t much light at the end of the tunnel.”
Coming out
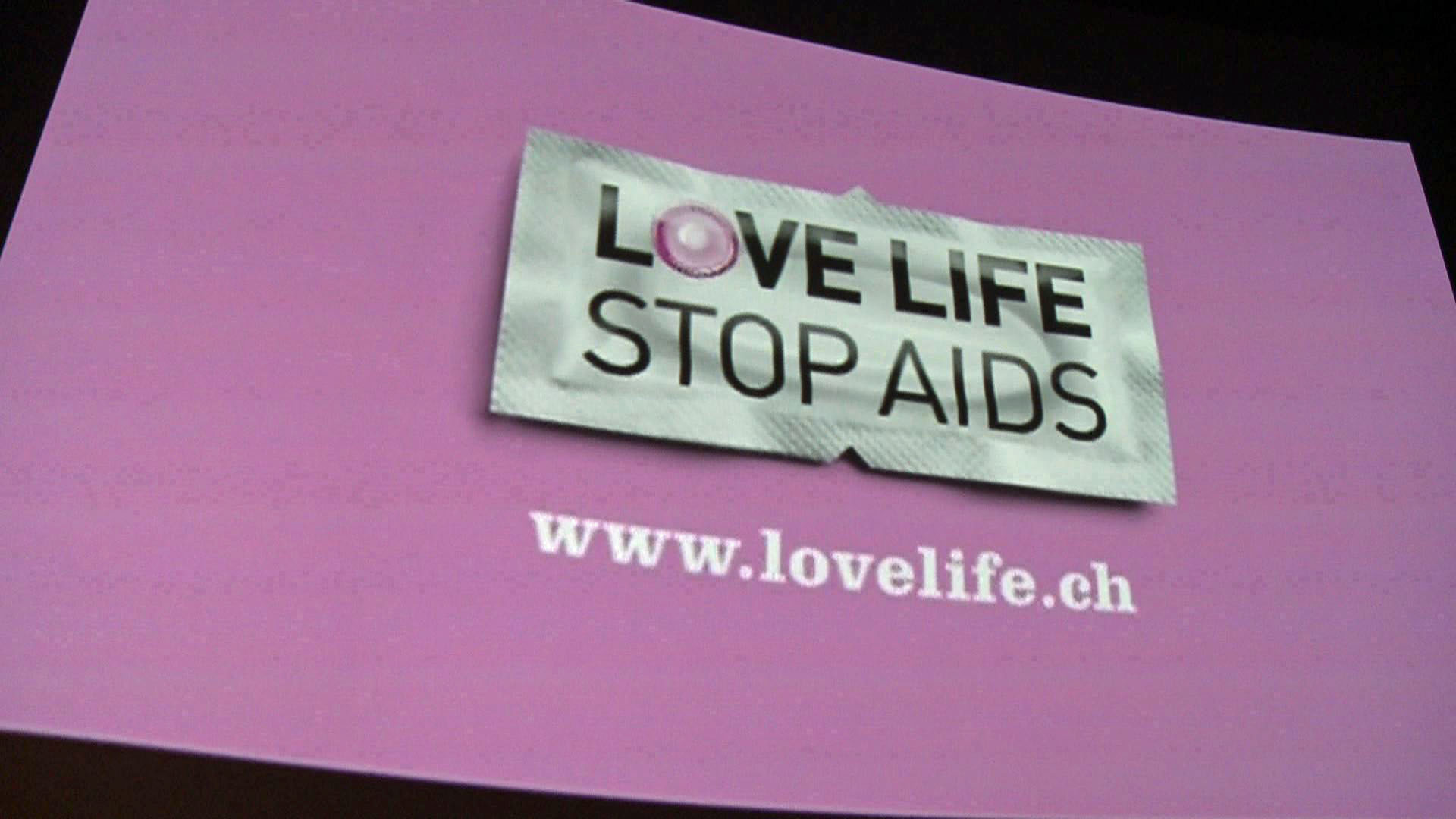
In Switzerland, HIV affects 0.4 per cent of the population – about 25,000 people. This is one of the highest rates in western Europe, despite prevention campaigns organised every year. Switzerland is the only country to have informed its population regularly since 1987, a year before World Aids Day was established on December 1.
Prevention works, insisted Harry Witzthum of the Swiss Aids Federation. “Today’s situation is linked to the history of the disease in Switzerland. Unlike other countries, we had to deal with three risk groups: the virus spread through homosexual men, drug addicts and migrants.”
This helps explain the number of new cases – 600 per year on average. “The level remains high, but since 2009 we have seen a decrease in infections in all the groups, thanks in part to prevention efforts,” said Witzthum.
The prevention message is addressed specifically to migrant groups. “Over 30 per cent of the heterosexual transmissions of HIV in Switzerland occur among migrants,” noted Witzthum.
For example, the number of infected patients is ten times higher than the national average among immigrants from sub-Saharan Africa, one of the most affected areas in the world.
Combating exclusion
In spite of medical progress, we still have a long way to go and we must not become complacent, recently warned health minister Alain Berset in Zurich.
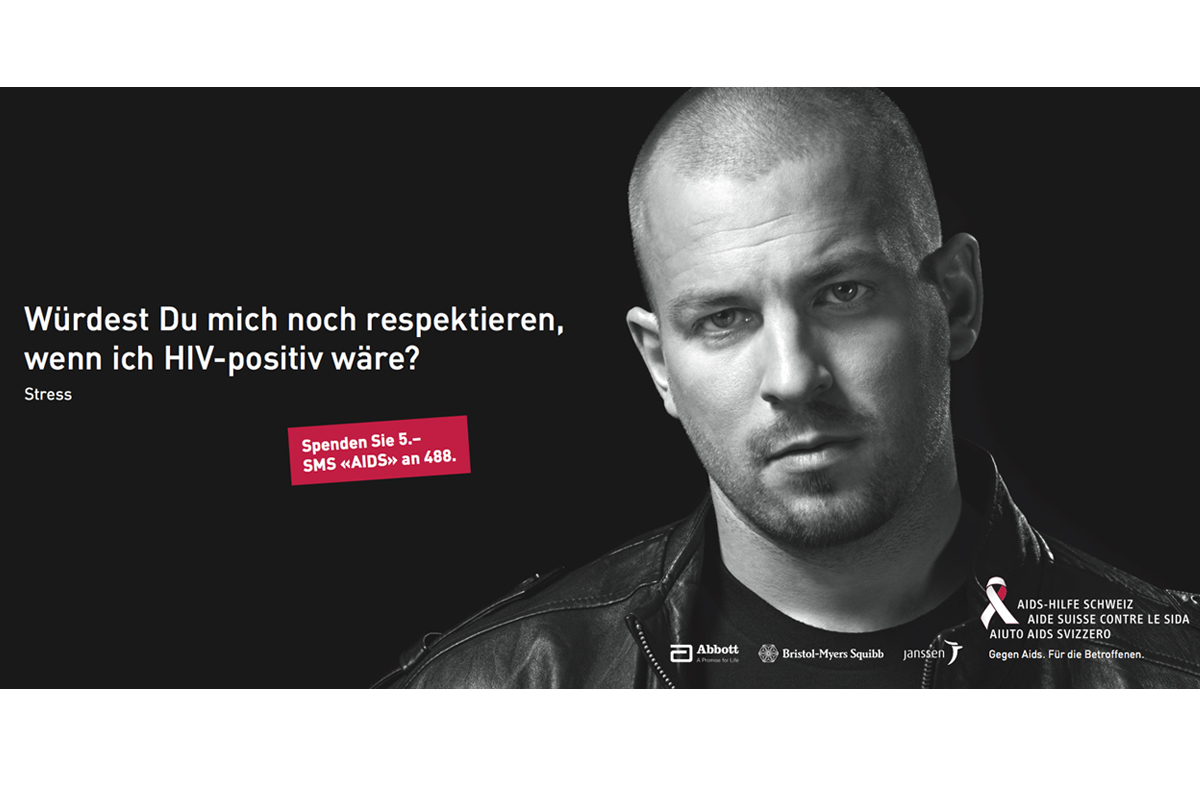
“A HIV diagnosis is accompanied by discrimination and stigmatisation, even in Switzerland,” said Berset.
On this front, progress has been slight, the Aids federation confirms, noting that the pain of feeling ostracised can lead to severe depression or even suicide.
During the first six months of the year, almost half the discrimination cases related to HIV brought to the attention of the organisation – 46 in total – were either work-related (unjustified termination or mobbing) or involved insurance companies.
“This is only the tip of the iceberg. We hear all the time of infected patients being disadvantaged in the workplace because of their disease,” noted Witzthum.
For the Aids federation, the struggle against the virus is still a struggle against exclusion from society, community and family.
Today a wide range of prevention tools is available and new approaches are being developed and to think of “a future generation free from Aids is no longer an utopian dream”, claimed the group. But this goal, it warned, cannot be achieved without first ending discrimination.
What is it? The human immunodeficiency virus (HIV), identified in 1983, weakens the immune defences of the organism. Present in body fluids (such as blood and sperm), it is the virus responsible for acquired immunodeficiency syndrome (Aids).
Where did it come from? It is believed that HIV comes from a virus found in some species of chimpanzees in West Central Africa.
How is it transmitted? Unprotected sexual relations; sharing of infected needles or syringes; transmission from mother to child during pregnancy, birth and breastfeeding, blood transfusions.
How does it act? HIV attacks lymphocytes, particularly those known as CD4 cells, and replicates itself within them. The organism reacts by producing antibodies, which are not able to eliminate the virus.
What are its effects? The number of lymphocytes goes down and the organism’s immune defences are progressively reduced. Aids is the final stage of HIV infection. At this point, almost any infectious agent, not usually pathogenic, can be life-threatening.
How is it treated? There are no drugs able to cure a HIV infection. There are drugs, however, that can prevent the virus from replicating. Usually treatments which involve different kinds of antiretrovirals (tritherapies) are the rule.
The number of people in Switzerland living with HIV or Aids is estimated at 25,000 (0.4% of the population).
The groups hardest hit are homosexual men and migrants from areas with a high incidence of the disease (Sub-Saharan Africa, South-East Asia, Eastern Europe and Central Asia).
About 11,000 people are receiving treatment. This treatment (covered by health insurance) costs on average SFr25,000 per person per year, resulting in a total cost of SFr260 million per year.
In 2011, 564 new cases were registered (759 in 2007). In the first seven months of 2012, there were 364 new cases.
Unprotected sex continues to be the main cause of trasmission of the HIV virus.
23.9% of positive tests done in 2011 involved women.
In 2011, there were 12 deaths due to Aids in Switzerland. In total, the disease has caused some 6,000 deaths.
(Sources: Swiss Aids Federation, Federal Health Office)
(Translated from Italian by Terence MacNamee)

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative


You can find an overview of ongoing debates with our journalists here. Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.