
A prescription written in your genes

Switzerland’s reputation as a research hotbed makes it a prime location for pioneering genetics-based medical technologies. We show how the multi-billion franc Swiss pharma industry is capitalising on these advances.
Given that all people are different, it makes sense that diseases – as well as the treatments for those diseases – affect each of us differently. That’s the logic behind precision medicine, also known as personalised, or data-driven medicine.
“The diversity with which cancer occurs in humans is infinitely larger than once thought,” says Silke Schneider, Managing Director of the Competence Center Personalised Medicine UZH/ETHExternal link in Zurich.
“I learned recently that there are probably as many cancer types as there are people on earth.”
Since the human genome was first sequenced in 2003, the combination of genetics with high-performance computing technology has made precision medicine a reality. By incorporating patients’ genetic information into their diagnosis and treatment, doctors hope to avoid much of the trial-and-error that still characterises aspects of modern healthcare – especially oncology.
“There is no such thing as ‘lung cancer’ – it doesn’t exist. Instead, there are thousands of different lung cancers,” says Jurgi Camblong, cofounder and CEO of Sophia GeneticsExternal link near Lausanne. The start-up from the Swiss Federal Institute of Technology Lausanne (EPFL) manages a network of over 80 hospitals across Europe that use a special software platform to analyse genetic data from patients, and provide diagnostic reports for doctors.
Pharma + genetics
Swiss pharmaceuticals
In Switzerland, the chemical and pharmaceutical industries generate about CHF79 billion ($82 billion) in exports annually. The industry employs about 65,000 people in Switzerland, and 355,000 worldwide.
Roche, Novartis, Merck, Serono, Syngenta, Firmenich and Givaudan are the biggest players in the Swiss pharma industry today, though the total number of companies in the sector totals nearly 1,000. The pharmaceutical sector in Switzerland has grown particularly since 2000, after the financial crisis and restructuring of the 1990s. Exports went from CHF8 billion in 1990 to CHF64.1 billion in 2012.
With its ten largest chemical and pharmaceutical companies comprising a CHF144 billion industry, Switzerland has much to gain from innovations in medical research, and particularly from those that can better match drugs to patients – a field called pharmacogenetics.
“The use of [genetic data] to develop more targeted drugs has been pursued by many Swiss pharmaceutical companies for years, and is important for the industry,” says Sara Käch of InterpharmaExternal link, Switzerland’s umbrella organisation representing research-based pharmaceutical companies. “Many new medicines are based on this approach.”
And indeed Roche and Novartis, the world’s top two providers of cancer drugs, have already integrated precision medicine into the big pharma business model: Novartis cites “precision oncologyExternal link” as a key element of its cancer drug portfolio, and in a recent interviewExternal link with Swiss newspaper LeTemps, Dietmar Berger of Roche stated that 70% of the company’s cancer drugs in the later stages of clinical testing have a genetic diagnostic test associated with them.
In 2015 alone, Roche spent $1 billion on a majority stake in Foundation Medicine, and acquired Kapa Biosystems – both United States-based companies that provide gene-sequencing tools – for its Personalised HealthcareExternal link Platform. Roche Diagnostics COO Roland Diggelman said in a statement that the acquisition of Kapa Biosystems built on Roche’s commitment to “provide our customers with a complete genetic testing solution”.
In June, both Roche and Novartis partnered with the US National Cancer Institute’s NCI-Match ProgramExternal link, a major clinical trial involving 2,400 US hospitals that will help match individual cancer cases with the precision drugs best suited to treat them.
Sophia Genetics CEO Jurgi Camblong is concerned that Switzerland and Europe lag behind the US in leveraging emerging genomic techniques into commercial success – at least when it comes to biotech start-ups requiring venture capital.
“The main difference between the US and Europe is that in the US, they are ready to go much faster, they have more money, they have higher ambition,” says Camblong.
“Technology is superior in Europe, but people tend to focus too much on the technology, and they expect it to be perfect before they will sell it. This is not the way it has to be done – the market tells you if the technology is right.”
For Camblong, the real value of precision medicine lies not just in drugs – but in the genetic data itself. Sophia Genetics’ software algorithm is based on machine learning, which means that as more hospitals join the network and contribute data, the more “experienced” the algorithm becomes, leading to more accurate diagnostics.
“If you are a doctor, and you detect genetic mutations in a patient, you may not know if these mutations are benign or pathogenic,” Camblong explains.
“Based on our information, you can make a decision and classify the mutation as, for example, pathogenic. The next time you, or another practitioner, find the mutation in a new patient, the software will tell you how it was previously classified. This way, you don’t lose the knowledge and effort of past work, and every other user in the network benefits from the information too.”
(Bio) banking resources
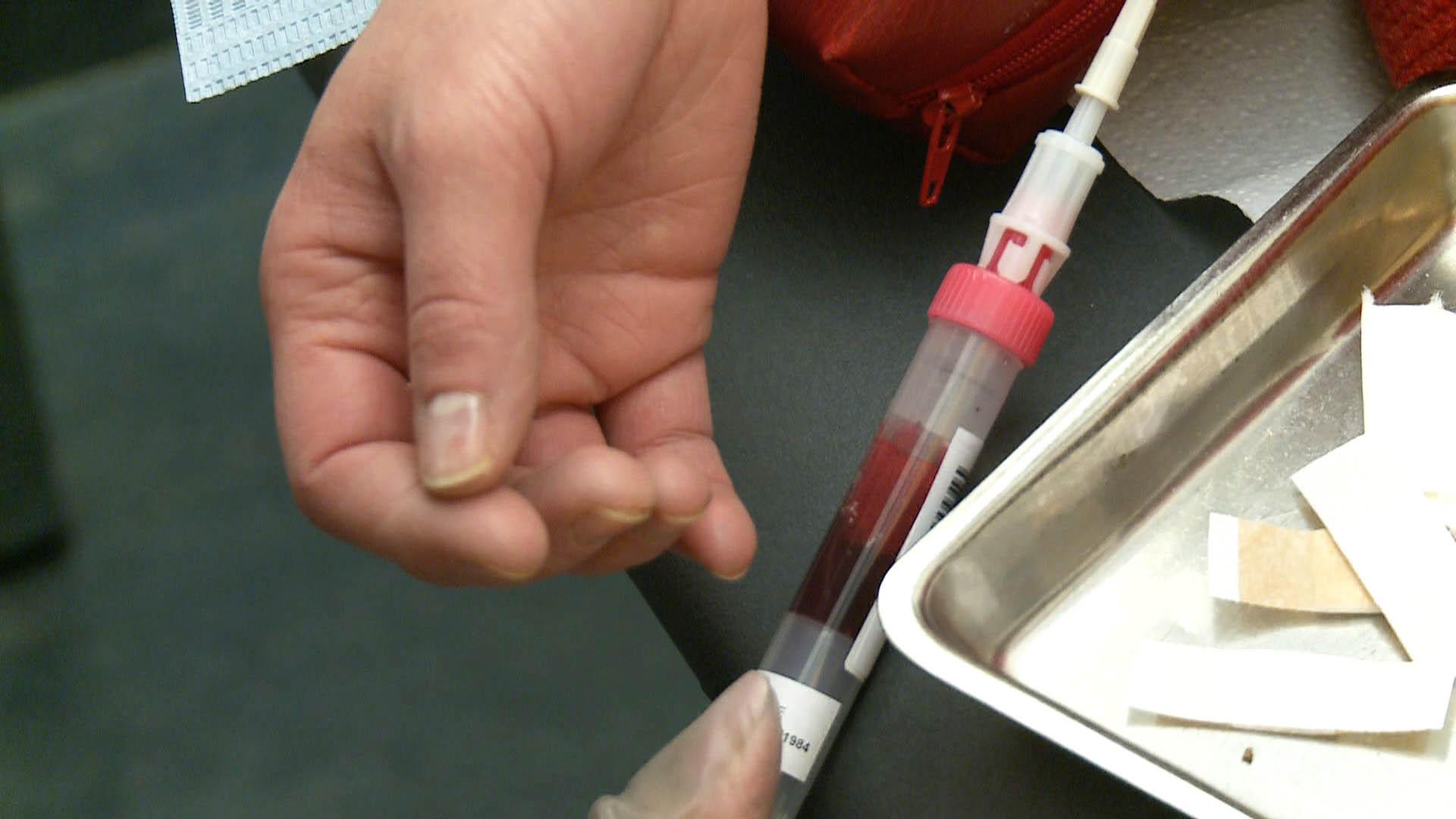
Vincent Mooser, the head of laboratories at Lausanne University Hospital (CHUV), spent a decade in the pharmaceutical industry before accepting a position as director of the Institutional Biobank of LausanneExternal link – Switzerland’s largest biobank.
Mooser says that the Lausanne biobank is “unique” because it combines consent-based data collection, protection, and clinical research into a single, integrated platform.
More
Lausanne’s biobank project is unique in Europe
“Our clinical support platform is, for me, a way to accelerate the discovery and development of new drugs,” he says, adding that the biobank has plans to partner with pharmaceutical companies to accelerate drug development.
Since 2013, the Lausanne biobank has been collecting DNA samples from CHUV patients. So far, 74% of patients who have been asked if they consent to having their genetic information stored in the biobank have agreed – amounting to DNA samples from nearly 21,000 patients.
“In the case of industries developing new drugs that might only work in a very small number of people – for example, drugs for a particular form of Parkinson’s disease – we can look at our database and find people who meet certain criteria, and ask them if they want to be part of a clinical trial,” Mooser says.
“We need new therapeutics and, given my experience on both sides, I see the opportunities to work with pharma from an academic perspective,” says Mooser. “I am convinced that we in Switzerland have an opportunity to partner in a mutually beneficial way with pharma to make an impact in precision medicine.”
Genetic data and privacy
Hacking, violation of privacy, and even potential discrimination against people with supposed genetic predispositions are all risks that accompany the sharing of personal genetic information. As precision medicine advances, data protection and ethical standards will also need to adapt.
Currently, at Sophia Genetics, raw patient data is not shared among hospitals – only information about how the data informs treatment decisions. At the Institutional Biobank of Lausanne, data are encrypted using special software developed by CHUV and EPFL. Patients contributing DNA samples to the biobank sign an agreement that allows researchers to use that data for any future project, on the condition that the research protects the patient’s personal privacy, and has been approved by a local ethics committee.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative





























You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.