
How less medicine could mean better health

Older patients are often excluded from clinical trials, with the result that much remains unknown about how they are affected by medications. Now, Swiss researchers are leading an EU-funded project to understand how to reduce the over-prescription of unnecessary treatments in the elderly.
“More than 60% of patients aged 65 and older admitted to the hospitals have polypharmacy,” says Nicolas Rodondi, a professor of internal medicine at Bern University Hospital, referring to the medical term for multiple drug prescriptions.
Some studies have found that roughly 30% of hospital admissions and 20% of unnecessary healthcare costs in the elderly are the result of duplicative, unnecessary, or otherwise inappropriate drug prescriptions.
“We find ourselves in a situation where lives last longer with every decade,” says Jürg Schlup, president of the Swiss Medical Association. “People also stay healthier thanks to improvements in the medical management of chronic diseases. It is here that we are confronted with the danger of over-medicalisation.”
Optimising therapy
Earlier this year, Rodondi and a team of experts from six EU countries responded to a call from the European Commission Horizon 2020 research framework to investigate the problem of over-medicalisation in the elderly. They received a total of €6.6 million in funding from the European Commission and from Switzerland’s State Secretariat for Education, Research and Innovation (SERI) to develop a software programme that will generate personalised medical recommendations for elderly patients.
The OPERAM study (OPtimising ThERapy to prevent Avoidable hospital admissions in the Multimorbid elderly) is the first health-oriented Horizon 2020 project to be led by Switzerland. It will focus on 1,900 patients aged 75 and older from all participating countries.
The researchers are developing software to identify medications that may be inappropriate for elderly patients, either because there is no specific indication for them, because they interact negatively with other drugs, or because an incorrect dosage has been prescribed.
The work could also reveal whether important medications are missing from a patient’s healthcare plan.
“We designed a trial to test whether a combination of interventions could not only decrease polypharmacy, but also improve clinical outcomes in the elderly – for example, by reducing the number of hospitalisations, and by increasing patient quality-of-life,” Rodondi explains.
Rodondi and his team hope that in addition to improving patient lives, the OPERAM project will save each participating country millions each year in healthcare costs.

More
The risks of overmedicating the elderly
Global issue
Rodondi is also involved in the direction of an initiative called smartermedicine.ch, which was established in 2014 under the direction of the Swiss Society of General Internal Medicine. Medical experts have developed a list of five procedures that Swiss doctors should avoid unless absolutely necessary, in the interest of improving patient wellbeing and avoiding “useless interventions”.
smartermedicine.ch’s top 5 procedures to avoid
1. A radiological assessment in a patient who has had non-specific lower back pain for less than six weeks
2. The PSA (prostate-specific antigen) test to screen for prostate cancer, without discussing risks and benefits with the patient
3. The prescription of antibiotics for minor infections of the upper airway
4. A chest radiograph during preoperative assessment, in the absence of any symptoms of chest pathology
5. The long-term use of proton pump inhibitors for gastrointestinal symptoms without using the lowest effective dose
The OPERAM project is intended to go a step beyond smartermedicine.ch by investigating how changes in medication affect the health of patients based on 18 different medical treatments.
How many pills a day?
Rodondi says that in Switzerland, over-prescription leads to many older patients taking as many as ten different kinds of medicine every day.
But how does this happen – isn’t it obvious when a medication or procedure isn’t needed? In fact, there are several common causes of polypharmacy, and the OPERAM project aims to address each of them.
Care coordination is one issue: treatments from general practitioners may not necessarily be harmonised with prescriptions from specialists, or those issued during hospitalisation.
Sometimes, the cause of over-medicalisation originates with the patients themselves; many of us feel more comfortable leaving the doctor’s office with a prescription slip, rather than empty-handed. For example, insomnia is a common complaint of older adults, and patients will often request sleep aids from their doctors. But side-effects of many sleep aids include dizziness and loss of balance, which can increase the risk of falls and serious injuries in older patients.
Rodondi says that the prescription of antibiotics for non-bacterial infections – such as a flu virus – is another common example.
“You can do two things – you can tell the patient they have a viral infection, and to go home, take some medication to decrease symptoms, and wait for it to disappear itself. Or, you can give antibiotics, and people are happy with the doctor. But then you have other problems, like more antibiotic resistance or side-effects,” Rodondi says.
Data adaptation
One reason for over-medicalisation is that there is still much that doctors do not know about elderly patients with more than one illness, and about how different interventions affect them. To make matters worse, such patients are often excluded from clinical trials, due to concerns that multiple conditions could distort the accuracy of trial results.
“Only 2% of clinical trials include people with more than one disease in a trial, even though this is 60% of people over age 65,” says Rodondi.
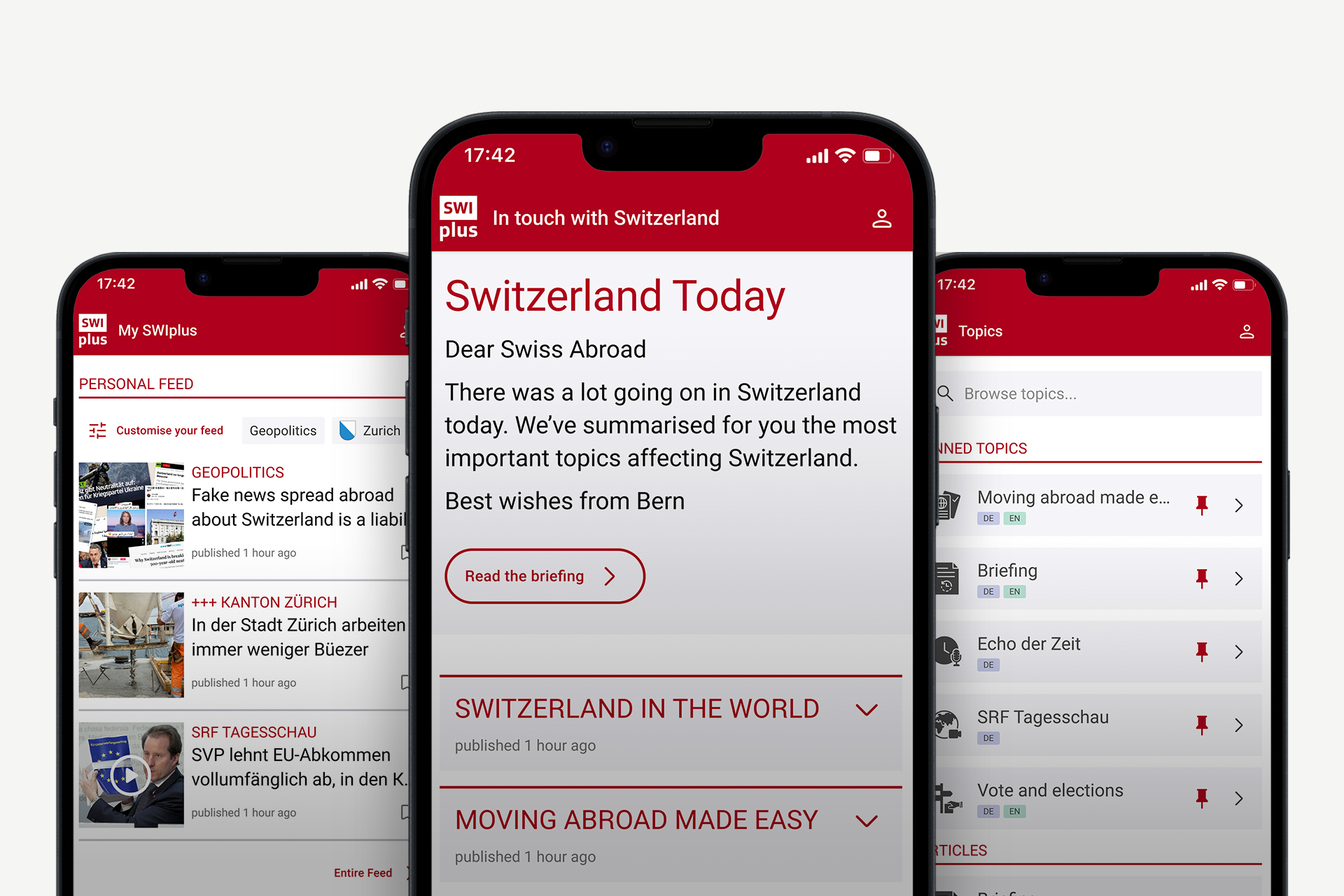
He adds that this lack of sufficient data is exacerbated by the fact that unlike other nations such as Denmark, Switzerland does not have a central healthcare data repository.
Instead, Swiss healthcare data is decentralised and kept separately by various medical or insurance institutions, making research coordination difficult.
In June, a CHF20 million National Research Programme (NRP) called “A health system better adapted to future challenges” was launchedExternal link to address this problem. One of the goals of the programme is to improve the availability, accessibility, and comparability of medical data.
An ageing population
Finding solutions to challenges associated with providing sound medical care to the elderly is especially important in industrialised countries like Switzerland where the population is ageing. In 2014, there were four Swiss between the ages of 20-64 for every one over the age of 65. In 1860, that ratio was 12 to 1.
The median age in Switzerland is increasing primarily because the birth rate is decreasing. Today, the average number of children per woman is about 1.5, compared to 2.5 in the 1940s and 1950s.
Part of the aging population phenomenon is also attributable to increased life expectancy, which has been rising globally over the last 50 years. The Swiss are some of the longest-lived people in the world: in 2014, the average life expectancy was 81 for Swiss men, and 85 for Swiss women.

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative



























You can find an overview of ongoing debates with our journalists here . Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.